Lung cancer
- Overview
Lung cancer is one of the most common types of malignant tumors and also one of the most common causes of cancer-related death. Lung cancer occurs in the bronchial mucosa epithelium, it is also known as bronchial carcinoma. The World Health Organization (WHO) divides lung cancer into four main types by histological classification: small cell lung cancer (SCLC), large cell carcinoma (LCC), squamous cell carcinoma (SCC) and adenocarcinoma (ADC).
Lung cancer gene detection is detection of lung cancer-related genes in samples of cancer tissue and peripheral blood through use of high-throughput sequencing platform. Through lung cancer gene detection, interpretation of lung cancer targeted drugs, detailed understanding of specific genetic mutations in lung cancer patients and personalized medication guidance for patients can be achieved.
- The Necessity of Genetic Testing
Tumor heterogeneity describes the observation that different tumor cells can show distinct morphological and phenotypic profiles, including cellular morphology, gene expression, metabolism, motility, proliferation, and metastatic potential. This phenomenon occurs both between tumors (inter-tumor heterogeneity) and within tumors (intra-tumor heterogeneity). Because of the heterogeneity of tumor, a same drug may have different effects on patients with the same type of tumor. For example, when the EGFR gene of lung cancer patients is wild-type, the effect of gefitinib (Iressa) and erlotinib (Tarceva) is not significant; when exon 18 of EGFR gene shows positive mutation, the effect of gephinib, erlotinib, and afatinib is significant.
Tumor often develops drug resistance. In the beginning of drug treatment, most cancer patients have good curative effect, which slows down after the genome of the tumor cells develops drug resistance. All lung cancer patients who carry EGFR mutations and use EGFR tyrosine kinase inhibitors (TKI) for treatment can acquire resistance to the drugs.
Suggestions are made in the lung cancer diagnosis and treatment guidelines of American Society for Clinical Oncology (ASCO), the lung cancer diagnosis and treatment guidelines of National Comprehensive Cancer Network (NCCN), European Society for Medical Oncology (ESMO), the primary lung cancer diagnosis and treatment standard stipulated by National Health and Family Planning Commission and other guidelines that patients with lung cancer should accept genetic testing before receiving targeted therapy.
- Testing Content and Medication Guidance
By using modern molecular biology techniques (high-throughput sequencing technology, gene chip technology, etc.), the genetic sequence of an individual can be detected, analyzed and compared with known lung cancer-related genes. Therefore, guidance on medication (which involves over 70 clinical drugs) can be offered to the individual.
|
Part of the genes for detection |
ALK BRAF EGFR HER2 KRAS MET RET ROS1 CDK4 CDK6 DDR2 FLT1 FGF19 FGR1 FGR2 FGFR1 FGFR2 HRAS KDR MKP2K1 NRAS NTRK1 NTRK2 PIK3CA PTEN RB1 RICTOR SRK11 TP53 TSC1 VEGFA PDGFRA PDGFRB PIK3CA |
|
Part of the targeted drugs |
Gefitinib, Erlotinib, Ekotinib, Oxazolidine, Alfatidine, Oxyetinib, Sertini, Alsette, Vanderbilt, Carbotinib, Virolinone, Dalafenib, Cetuximab, Trastuzumab , Bevacizumab, Everolimus, Aolapani, Quimeitidine, Tenitroxicam, Sorafenib, Erlitinib, Avitinib, Lenapine, Sixtemidine, Erlitinib AZD2014 AZD4547 AZD1775 BGJ398 BYL719 EGF816 INC280 |
|
Major manufacturers |
Roche Betta Pharmaceuticals Co., Ltd Pfizer Novartis GlaxoSmithKline |
|
Notes |
The drugs listed here include FDA/CDFA-approved drugs and clinical trial drugs |
- Applicable People
Lung cancer patients who expect to adopt targeted drug therapy
Lung cancer patients who wish to replace a poor therapy with an effective new one
Lung cancer patients who need new therapy because of drug resistance, recurrence or metastasis of the cancer
- Clinical Significance
Genetic testing can help lung cancer patients select appropriate targeted drugs and can detect acquired drug resistance mutations.
- Sample Requirements
Fresh cancer tissue: ≥60mg
Fresh percutaneous biopsy tissue: 2~3 needles
Paraffin-embedded tissue: 8~10 paraffin embedded tissue sections
DNA: concentration≥30ng/μL, 260/280≈1.8~2.0,gDNA≥1ug,cfDNA≥500ng
Peripheral blood: 10mL fresh peripheral blood
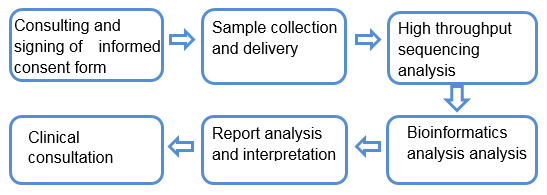
- Service Process
- 上一篇:Breast cancer
- 下一篇:
